Recently, a term called “COVID prone positioning”has been discussed a lot on the Internet, for example,“Remember this life-saving position!”, “The prone position can improve hypoxia”, “The elderly with breathing difficulties should sleep with this position”. There are also many questions raised: Is this true? How can lying in the prone position save lives? Can old people with underlying diseases try this method? Professional rehabilitation therapists from DeltaHealth Hospital will answer these questions for you.

Question 1: What’s “COVID prone positioning”? Can it really save lives?
Answer: Yes! Prone position can really save lives!
According to the therapists from DeltaHealth Hospital, the so called “COVID prone position” online is actually prone ventilation, a lung protective strategy commonly used in ICU. It uses turn-over bed or device, or hand to help patients lie down in the prone position for breathing or ventilation. This method can effectively improve the ventilation/perfusion ratio, reexpand the dorsal collapsed alveoli, improve the flow of pulmonary and endotracheal secretions under gravity, and reduce the compression of the heart and mediastinum on the lung.
Question 2: Why “lying down” can facilitate breathing?
Answer: A person's lung is composed of small balloon like alveoli, and different positions will affect the “work efficiency” of the alveoli.
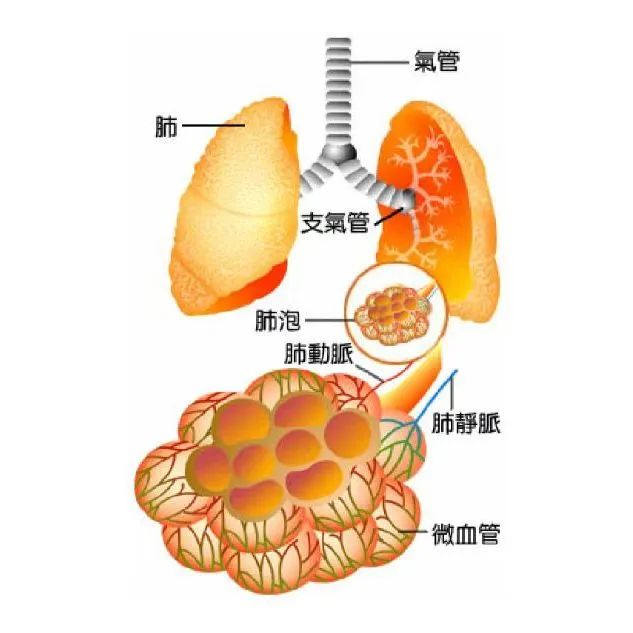
When you are in the "supine position", many small balloons (alveoli) are collapsed and stop working, and there is only blood, without gas. And you will have hypoxia, chest distress, wheezing, palpitation and other discomfort symptoms...
When you take the “prone position”, your back is shifted to the top, and the alveoli are no longer pressed. Oxygen can be inhaled, carbon dioxide can be exhaled, and the small balloons return to work! Then there is both gas and blood in the lungs. As the ventilation-perfusion ratio is more balanced, breathing becomes easier. And because of gravity, sputum is easy to cough up.
Question 3: What should you pay attention to when using prone ventilation at home?
1. Stop eating 1-2 hours before prone ventilation;
2. 3 pillows are needed; put the first pillow under your arm, the second under the hip, and the third one at the position parallel to lower leg; Pregnant women, obese patients, and those with abdominal wounds had better empty their abdomen to avoid pressure, or take the lateral position;
3. It can be carried out in different periods within a day, 1-2 hours each time, and 12 hours per day is recommended.
4. Relax the body, do not use the strength of elbow or shoulder, avoid plank or push-up posture;
5. Pay attention to the indoor temperature, prevent patients from wearing too thick clothes;
6. Reserve space for oxygen tube and mask for convenient adjustment and observation.
DeltaHealth Hospital kindly reminds you: if the patient’s discomfort is still not relieved and SpO2 is lower than 93% after taking prone ventilation, it is necessary to seek medical advice in time.
Although prone ventilation can relieve related symptoms, it is not suitable for everyone!
Who should not do prone ventilation?
Prone ventilation is not suitable for everyone. For the following groups, conditions may worsen after they take prone ventilation.
1. Critically ill patients with severe hemodynamic instability
2. Patients having craniocerebral trauma with moderate and severe intracranial hypertension
3. Patients with acute hemorrhagic diseases
4. Those having severe multiple injuries with severe damage to the cervical vertebra, spine, pelvis, chest wall and abdomen
5. Those that have severe facial trauma or undergone recent facial surgery
6. Patients receiving tracheal, sternal, or orthopedic surgery recently
7. Patients having recent abdominal surgery
8. Patients having pacemaker implantation recently (within 2 days)
9. Patients receiving DVT treatment for less than 2 days
10. Those having even worsened oxygenation indicator after taking prone position
11. Patients with ventricular arrhythmia
Apart from prone positioning, is there any other method to relieve shortness of breath?
1. Sloping side-lying position: use several pillows to support the upper part of the body, the head and neck, to lie on one side, with knees slightly bent.

2. Lean forward: sit at a table, lean forward from the waist up, put head and neck on the pillow, and put your arms on the table. Or try lying on your arms without using a pillow.

3. Lean forward (no table) : sit in a chair, lean forward, and place your arms on your knees or on the armrest.

Learn two breathing methods
1. Controlled breathing technique
a. Keep a comfortable sitting position with sufficient support.
b. Place one hand on your chest and the other on your abdomen.
c. Close your eyes (otherwise keep them open) and focus on your breathing, only if it can help you to relax.
d. Breathe gently in through your nose (or your mouth when you can’t) and out through your mouth.
e. When breathing in, you will feel that the hand placed on the abdomen rises and falls more obviously than the hand placed on the chest.
f. Try to breathe slowly, easily and fluidly.
2. Rhythmic breathing
a. This method can be used when you are doing activities that require much physical strength or cause shortness of breath (such as climbing stairs or hills) :
b. Try dividing an activity into smaller ones to make it easier to complete without feeling tired or out of breath.
c. Inhale before performing the strenuous activity, such as going up a step.
d. Exhale during exertion, such as climbing a step.
e. It helps to breathe in through the nose and out through the mouth.
Do not rush into completing the strenuous activities, and rest properly.
During the recovery, what kind of symptoms need immediate medical treatment?
When you recover from COVID, some complications that require immediate medical treatment may occur. If you have any of the following dangerous symptoms, please contact health professionals and go to the hospital immediately!
1. Obvious shortness of breath occurs after slight exercise, which could not be improved by taking postures used to relieve shortness of breath;
2. The degree of shortness of breath changes at rest, and can not be improved by controlled breathing technique;
3. Chest pain, tachycardia, or dizziness occur when taking certain postures, activities, or exercises;
4. Having confusion which exacerbates, or difficulty speaking or understanding others;
5. Weakness of the face, arms and legs, especially on one side of the body;
6. Having anxiety or bad mood, or thinking about hurting yourself.
References:
[1]康复指导手册:COVID-19相关疾病的自我管理(第二版)
[2]新型冠状病毒肺炎患者俯卧位治疗上海专家建议
[3]新型冠状病毒肺炎诊疗方案(试行第十版)